What is Hyperhidrosis?
Essential hyperhidrosis (EH) typically targets the armpits, palms of the hands and the soles of the feet, where the sweat gland density is highest. There are 2–5 million eccrine sweat glands on the skin surface that can secrete at a rate of 3–4 litres per hour, so hyperhidrosis sufferers are literally dripping with sweat. Usually one location (either the armpits or palms/soles) tends to be the predominant site. Hyperhidrosis studies have not identified any sweat gland pathology nor any changes in sweat gland sensitivity to autonomic stimulation. There is however increased neural stimulation of the target sweat glands signalling increased sweat output. Consequently baseline sweating is increased, worsens with emotional stress, and only stops during sleep. By contrast, secondary hyperhidrosis can result from chronic illness, endocrine and metabolic disorders (e.g. thyroid, diabetes, menopausal), infection, malignancy (lymphomas), medications, and an important point of difference is that secondary hyperhidrosis does not stop during sleep. Although armpit hyperhidrosis is usually not malodorous, patients tend to feel extremely self-conscious about the constant dampness and may actively avoid socialising or forming close relationships. Secondary anxiety and depressive disorders are common with hyperhidrosis. Palm hyperhidrosis affects grip and interferes with handling of paper documents (soaked) and keyboards (slippery). Feet hyperhidrosis in occlusive footwear predisposes to maceration and secondary fungal and micrococcal skin infections and may become malodorous.
How can Hyperhidrosis be treated?
Topical aluminium chloride (Driclor AlCl) is the first-line treatment for most cases of hyperhidrosis especially for the armpit region. The AlCl blocks the sweat ducts to decrease the sweat output. The lotion is applied to the affected area before bedtime every night (washed off in morning) for the first week then maintained at once or twice a week. Potential skin irritation and lack of efficacy (in palms and soles) are the limiting factors. Oral anticholinergic agents (e.g. Pro-Banthine) can be useful for hyperhidrosis, especially generalised hyperhidrosis. Unfortunately at therapeutic dosages, many patients are unable to tolerate the predictable anticholinergic effects of dry mouth, blurred vision and urinary retention. Iontophoresis involves soaking hands and feet in tap water that is charged with a weak electric current. Affordable home devices are now available for convenient self-administration. A typical schedule is 20 minutes, three times a week for the first six weeks followed by weekly maintenance. Anti-wrinkle injections have gained widespread acceptance as an effective option for localised hyperhidrosis. They are administered through multiple injection points at each site and can stop sweating for 6–9 months. Transient weakness in grip can occur when treating the palms. The recurring cost (without PBS subsidy) is a potential barrier. Anti-wrinkle product treatment can be administered under the PBS indication for armpit hyperhidrosis in patients who have failed topical AlCl. Surgical options such as sympathectomy and sweat gland liposuction/ excision are considered in refractory cases. Endoscopic sympathectomy involves cutting the appropriate ganglion to stop innervated sweating (T2 for face, T3 for axillae and hands). Side effects include compensatory sweating elsewhere, Horner’s syndrome (thoracic sympathectomy), pneumothorax and sexual dysfunction (lumbar sympathectomy).

Download the “Hyperhidrosis” article
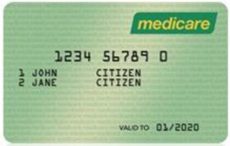
Medicare rebates apply.
Since 2013, Medicare has approved PBS subsidy of anti-wrinkle injections for excessive sweating of the armpits. Patients must have tried and failed the anti-perspirant DRICLOR. Patients are allowed to have treatment every 19 weeks or longer.